|
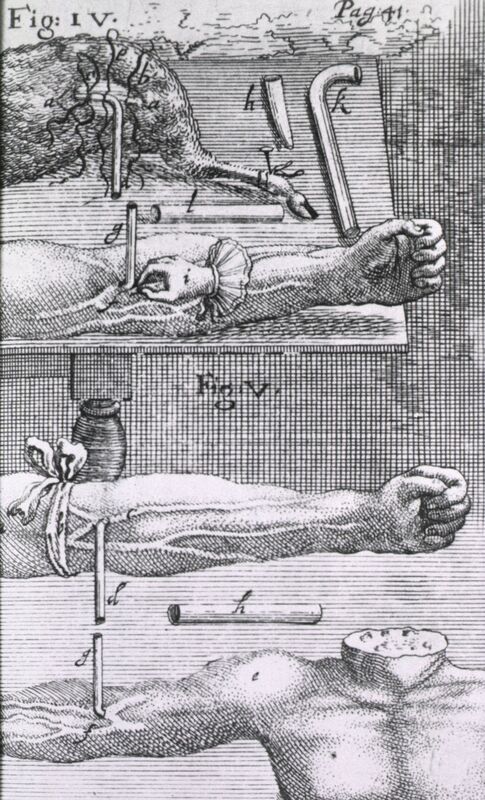
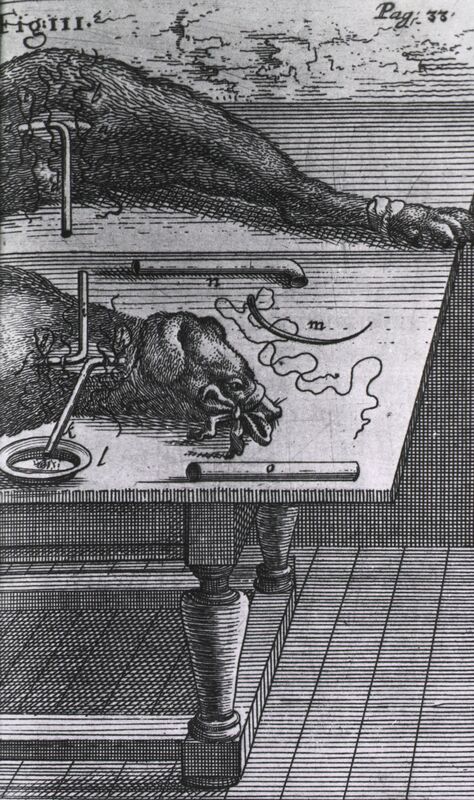
Nearly 18 million blood transfusions are done in United States hospitals each year, saving the lives of new mothers who lose blood during childbirth, people who suffer from traumatic injuries, premature babies with anemia, and more. The average hospital patient pays $219 for just 16 ounces. Blood truly is life-saving and precious. But there was a time when blood transfusions were viewed with suspicion and were eventually banned - for more than a century - in many parts of Europe. Transfusions were first attempted in the mid-1600s, a time when medical science in Europe was still deeply entrenched in the teachings of Galen, the famous Greek physician. At that time, surgical exploration was done only on the dead, and only on criminals who were charged with capital punishment. In the 15th century, Pope Sixtus IV officially sanctioned the dissection of criminals, partially as a way to punish them even after death. With only deceased criminals on the surgical table, physicians were limited in what they could learn. Galen taught that blood originated from digested food, was filtered by the liver, and then sent to the heart where it seeped through invisible pores. The heart’s job was to burn blood, and respiration was the body’s way of blowing off the smoke produced by the heat of the heart’s furnace. Blood was still a mysterious fluid. A few decades earlier, English physician William Harvey shocked the medical community by discovering that blood circulated throughout the body. Bloodletting was a popular treatment and thought to cure most everything, particularly fever, which was a sign of too much blood, according to the dogma of the day. The idea of transfusing blood into a body was contrary to the science of the day, and viewed as misguided and ghastly. In a time where bloodletting was the European physician’s go-to procedure for nearly all ailments, transfusions were unheard of. But one English physician was ready to change all of that. The First Blood Transfusion Richard Lower performed the first animal to animal blood transfusion in 1666, sanctioned by London’s Royal Society. He used dogs, tied them down, and performed the procedure with no anesthetic. The dogs howled in pain, but Lower and his team paid no attention, believing at the time that animals had limited ability to feel pain and emotion. Using hollow goose quills to puncture arteries and veins, and silver tubes to transfer the blood, Lower bled one dog nearly to death, then transfused it directly from a healthy dog, savings its life. Blood had been tricky to work with – it clots when exposed to air – and Lower was the first to solve that issue by using tubes to transfer it. His experiments were delayed by outbreaks of the plaque and the Great Fire of London in 1666, but he pressed on and eventually published his work. The First Blood Transfusions on Humans Jean-Baptiste Denis, a French physician, read Lower’s paper and decided to copy his technique using humans. His first patient was a teenage boy who suffered from extreme fevers. He transfused three ounces of lamb’s blood into the boy. The animal was chosen because of its Biblical meaning; they are viewed as calm, and the boy was not. The purity and tranquility of the lamb was expected to be transferred, along with the blood, to the boy. Denis was pleased to find that it worked. Other than a feeling of heat in the transfused arm, the boy recovered. Excited by his apparent success, Denis kept going. A local butcher who was known as an alcoholic signed up to be Denis’ next guinea pig. Records show that after the transfusion, the patient butchered the donor lamb, then celebrated by getting drunk. Another patient was a man with liver disease. Denis used calf’s blood and reported that the man’s condition improved. Transfusion and Murder
Antoine Mauroy was a 34-year-old man who suffered bouts of insanity. The episodes would last for months, during which he would beat his wife and run naked throughout Paris, setting things on fire as he went. Local physicians had tried many unsuccessful treatments. One day, a good samaritan found him and, thinking he was homeless, brought him to Denis, as his wife wandered through Paris looking for him. Denis removed ten ounces of his blood and replaced it with the same amount of calf’s blood. Mauroy improved slightly and was transfused again two days later. This time, his body reacted badly. His urine turned black, and he vomited, had a high fever, and began sweating profusely. After a few days, he improved, went home, and apparently became a loving husband with no sign of mental illness. Later, he regressed. His wife Perrine brought him back for another transfusion, hoping it would cure his insanity once more. He may or may not have been transfused a third time, but we know he died the next day and Denis was arrested for murder. Denis argued that he was preparing for the third transfusion but stopped when Mauroy had a seizure. During the trial, witnesses claimed they saw someone pay Perrine to kill her husband with poison – most likely a physician who was against blood transfusion. Another witness said the Mauroy’s cat died after drinking broth Perrine had prepared for her husband. Perrine was executed and Denis walked free. While the witness’s stories may seem far-fetched, Perrine did seem to come into some money – after a lifetime of poverty, she somehow paid for the calf and transfusion, and her husband’s coffin, grave, and gravedigger. Historians think that a group of physicians, outraged at Denis for performing blood transfusions, paid Perrine to kill her husband in order to stop the practice for good. It worked. Pope Innocent XI banned blood transfusions, followed later by the French and English governments. The ban wouldn’t be lifted for over 100 years. Why Did Those Transfusions Seem to Work? Today, we know that transfusing blood from one species into another causes an intense immune reaction. In 1901, Austrian scientist Karl Landsteiner discovered blood groups, helping us understand blood science further. But Mauroy did improve after his transfusions – how? Some historians think that Mauroy’s psychosis was the result of tertiary syphilis – an advanced stage of syphilis that causes dementia and personality changes. Transfusing a patient with the wrong type of blood causes an immune reaction in the body, which usually includes a high fever. We know now that Treponema pallidum, the bacterium that causes syphilis, is sensitive to high temperatures. Mauroy may have been temporarily “cured” of his syphilis if the high fever killed off the bacteria. In the 1920s, an Austrian physician named Julius Wagner-Jauregg proved that syphilis could be treated with fever therapy. He put patients in a fever cabinet or purposefully injected them with malaria until the fevers killed the syphilis bacteria. Before his patients died of malaria, he saved them with quinine. As for the other patients who seemed to be cured from lamb or calf blood transfusions, historians think the amount of blood – usually just a few ounces – was not enough to cause an overwhelming immune reaction. If large amounts of the blood of another species were transfused, they most likely would have died since the immune system attacks foreign blood. This is called a hemolytic transfusion reaction; it causes bloody urine, fever, pain, and sweating – all symptoms that Antoine Mauroy experienced. The reaction he had to the transfusions raised his temperature enough to kill off the syphilis bacteria, but eventually his immune system response - or the possible poisoning - spelled the end for him.
1 Comment
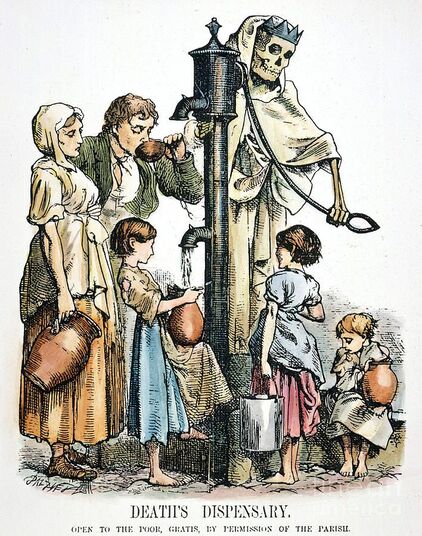
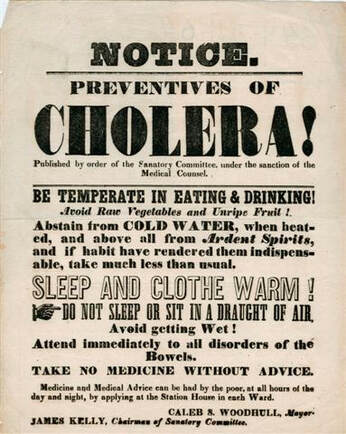
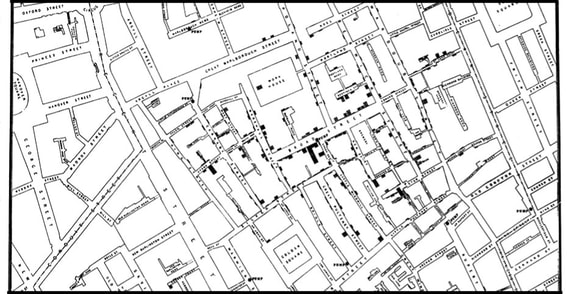
By: Courtney Southwick This past summer, my husband and I took a trip to England to celebrate our anniversary and my graduation from my master's program. Being a health science major, I was excited to see the Broad Street pump in London. In fact, that was our first stop after we flew into Heathrow! We drove through the awful London traffic to see the pump. That spot is very exciting to me because it is the birthplace of the field of epidemiology. It’s the spot where in 1854 a physician named John Snow tracked down the source of a cholera epidemic and changed the future of medical science. Cholera was very common in London at the time. It is an acute diarrheal illness caused by the Vibrio cholerae bacterium. It is spread through the fecal-oral route, meaning people become infected by ingesting contaminated food or water. The symptoms can be severe: watery diarrhea, vomiting, rapid heart rate, and extreme dehydration of the body. The loss of fluid happens so quickly that death usually comes within a few hours. There were cholera epidemics every few years in 19th-century London and each time, thousands died. The idea that germs caused disease was very new and not widely accepted during this time. Microscopes were also very uncommon so there was no way to see the cholera bacterium. London’s poor sanitation and open slaughterhouses created a putrid smell in the air. At the time, most people assumed that the bad air, or miasma, was the cause of disease. Dr. John Snow was the only person who suspected that cholera came from the water supply. Most Londoners got their water from community street pumps. Dr. Snow interviewed survivors and found that their symptoms always started in the gastrointestinal tract. He thought that if it was caused by miasma, the symptoms would be pulmonary. He published a paper blaming it on the water, and no one took him seriously. The idea of invisible microbes infecting water and causing sickness was an outrageous idea for its time. During a particularly bad outbreak in Westminster, Dr. Snow went door to door interviewing hundreds of family members of cholera victims. Almost all of them said the victim had gotten their water from the Broad Street Pump. He felt that this confirmed his theory and asked the Board of Guardians to remove the pump’s handle. The Board did not take him seriously. It took a lot of convincing, but eventually they agreed to remove the handle, just in case he was right. The intervention worked. Soon after the pump was disabled, cases of cholera decreased dramatically. Dr. John Snow revolutionized medical science. He was the first to track down the cause of an illness and produce a hypothesis for transmission of a disease. He was the first to systematically investigate cases and propose an intervention – removing the pump handle – which prevented further cases. None of this had ever been done before. He created the field of epidemiology and his work is still highly regarded today.
My husband and I visited the pump on a weekend evening in June. People were drinking inside the aptly named John Snow pub nearby and spilling out onto the sidewalk. At the pump, backpacks and jackets were piled up as people stood nearby drinking and chatting. I began to take a few pictures when a group of men noticed and cleared the area of their belongings. They stared, curious as to why I was taking pictures of a defunct water pump. One man stopped me and asked, “Why do people keep taking pictures of this pump?” Being a student of epidemiology, I struggled to keep my explanation short. As I told him the significance of the pump, his friends leaned in to listen. After my story, one of them said, “Wow, we’ve been coming here for years and had no idea!” Together, the group raised their cups of beer and cheered, “To John Snow!”
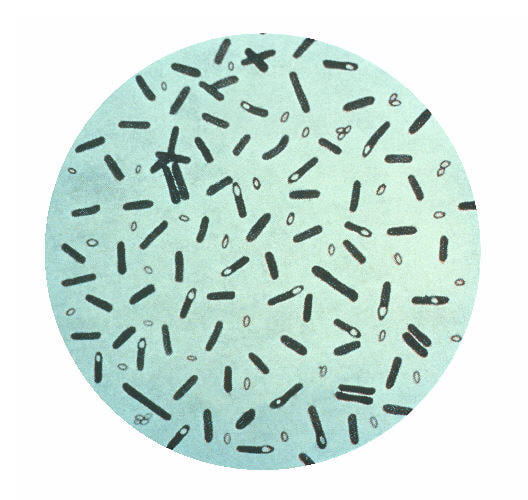
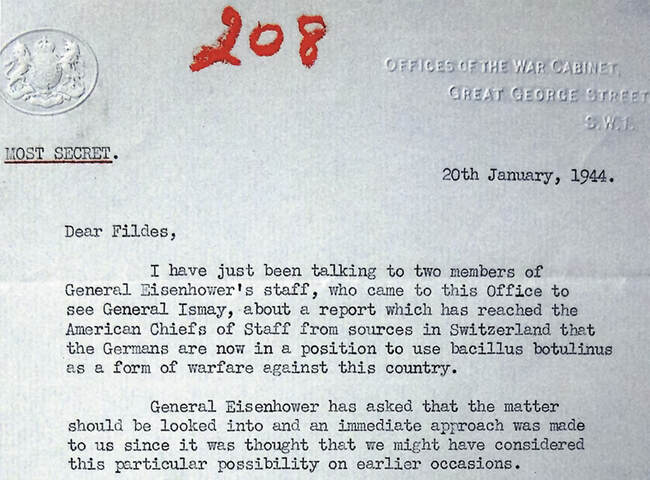
Given how deadly the toxin is, it may be surprising to learn that it has legitimate medical uses. A purified form of the toxin is used in the cosmetic procedure called Botox. Exceptionally small particles of the toxin are injected into the face to relax the muscles and reduce wrinkles. Botox is the most well-known procedure, but there are 5 types of Botulinum toxin that have been FDA-approved to treat twenty-five health conditions. These include crossed eyes, muscle stiffness, excessive sweating, chronic migraines, overactive bladders, and much more. The toxin is so strong that a tablespoon could provide the world’s medical and cosmetic supply for an entire year. The Early History Botulinum toxin has a long history. Writings from ancient Greece tell of a sickness that caused paralysis, vomiting, spasms, and respiratory failure. The culprit was poorly processed sausage contaminated with botulinum toxin. In the early 1800s, Dr. Justinus Kerner, a physician and poet, published the first case study of botulism, also caused by improperly prepared sausage. He documented the signs and symptoms, performed animal studies, and even experimented on himself. He was the first to recognize that the toxin interrupted motor signal transmission and he was the first to hypothesize about the therapeutic uses of the toxin. Emile Pierre-Marie van Ermengem, a bacteriologist in Belgium, made some breakthroughs as well. In the late 1800’s, Dozens of musicians fell ill after sharing a meal. Dr. van Ermengem studied the food they ate and found that the sick musicians had all chosen to eat ham at the dinner. The doctor isolated the bacterium and named it Bacillus botulinum, from the Latin word botulus, meaning sausage. Though many types of foods can cause botulism, the disease was strongly associated with sausage by that time. World War II Because of its extreme toxicity, botulinum toxin was eyed as a possible biological weapon during World War II. Allied intelligence sources wrongly reported that the Germans were working with botulinum toxin as a biological weapon. The report specifically stated that the Germans were preparing to use the weapon during Operation Overlord, the Battle of Normandy, which launched the Allied invasion of Europe. The reports eventually were found to be false, but it launched a years-long scientific endeavor in both England and the United States. Scientists at Porton Down in England and Camp Detrick (now called Fort Detrick) in the United States were tasked with purifying the toxin to create a bacteriological weapon. The weapon was only to be used as a defensive measure against the Nazis. At Porton Down, they studied the toxin throughout World War II. They had difficulty producing batches in mass that were consistent in their toxicity. They experimented with animals but had varied and disappointing results. The scientists were working toward two goals: to put the toxin into food and to coat the inside walls of bombs. The results were discouraging. The toxin in the food couldn’t be replicated consistently and the heat of the bombs decomposed the toxin. Research at Camp Detrick wasn’t much better. President Franklin D. Roosevelt approved the research, but only to be used in retaliation after the Nazis’ deployed their bacteriological weapon. He put George W. Merck, chemist and president of the pharmaceutical company Merck, in charge. Secret work on botulinum toxin weapons began in various universities across the United States. The main center of work was at Camp Detrick, where they succeeded in creating a purified, crystalline form of the toxin. This stabilized the toxin and prevented it from becoming degraded. The Americans discussed the possibility of creating an antidote to the toxin, called Toxoid X. The antidote would be the actual botulinum toxin treated to destroy its toxicity and retain its antigenicity. In other words, it would stimulate an immune response like a vaccine, but the soldiers would not fall ill. The plan was to immunize 1.5 million Allied soldiers. New British intelligence reports then produced irrefutable evidence that the Germans did not have the ability to produce biological weapons with botulinum toxin, so plans to inoculate the soldiers were dropped. On D-day, the soldiers who landed on Normandy beach carried gas masks for chemical attacks, but not biological attacks. As the war progressed, the truth became known. The Nazis had indeed been working on biological weapons, but with mustard gas and anthrax, not botulinum toxin. Hitler also banned offensive biological weapons but assigned German scientists to study them for defensive purposes. Heinrich Himmler, a top Nazi military leader, circumvented official orders and quietly gave authority to some labs to begin research into offensive bacteriological weapons. He also ordered experiments on concentration camp inmates. Botulinum Toxin Today
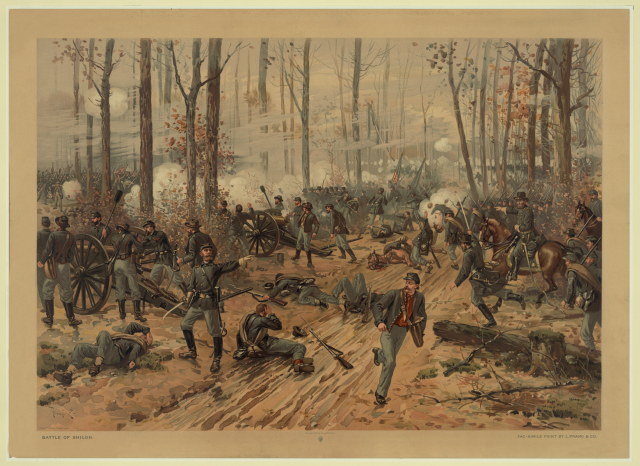
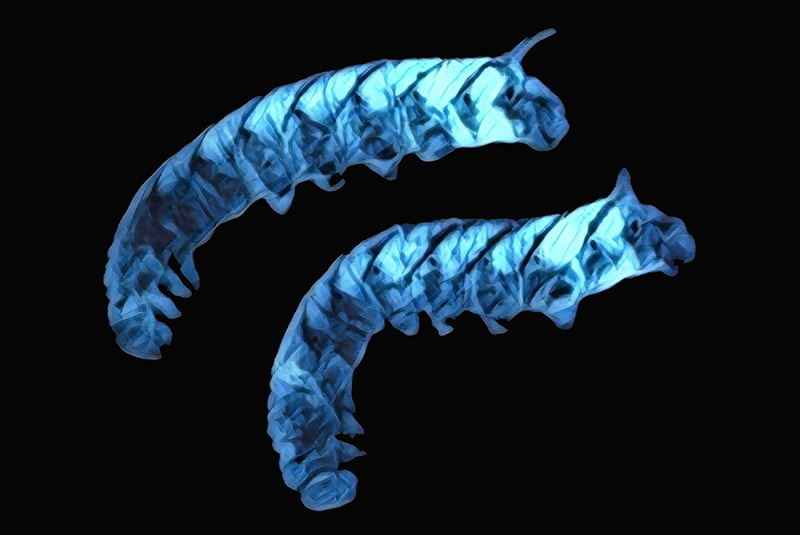
Years of research on botulinum toxin during the war concluded with an understanding that it is ineffective for weaponization. That pursuit was put to rest, but the research led to the purification of the toxin and paved the way for many medical uses today. The first official medical use was for strabismus, or crossed eyes. Alan Scott, an ophthalmologist was looking for an alternative to surgery for his patients. Botulinum toxin is a localized drug; it stays in one place instead of spreading throughout the body. Dr. Scott experimented with injecting the toxin near the eyes, which relaxed the muscles and allowed the condition to improve. He named his product Oculinum. It was approved by the FDA in 1989 for strabismus, blepharospasm (uncontrolled eye twitching), and other nerve disorders. The product was eventually sold to a company named Allergan, which changed the medication name to Botox in 1991. Jean and Alister Carruthers, an ophthalmologist and dermatologist in Canada, noticed their patients treated for blepharospasm had resolution of their frown lines after treatment. They published their findings in 1992 which led to many scientists conducting clinical trials to study the safety and efficacy of using botulinum toxin to reduce wrinkles. Eventually, the FDA approved it to treat moderate to severe glabellar lines, or forehead wrinkles, in April 2002. Since then, Botox has been used to decrease facial wrinkles, but also so much more. It was approved to treat abnormal head positions and severe neck pain associated with cervical dystonia, a very painful movement disorder. The toxin is also used as a treatment for facial asymmetry caused by facial nerve paralysis. The list goes on. Because of the clandestine work of military scientists, purified botulinum toxin has helped countless people relieve their pain and live normal lives. By: Courtney Southwick In April 1862, one year into the Civil War, Union General Ulysses S. Grant and his troops were deep in Confederate territory near the Tennessee River waiting on more troops to join them. They were camped outside of Shiloh, Tennessee at Pittsburg Landing. The soldiers were exhausted from months of marching and inadequate food portions. The stress was high, and the living was unhygienic. As a result, the soldiers’ immune systems were struggling. On April 6th, before the additional Union troops had arrived, the Confederates launched a surprise attack on Grant and his troops. The fighting continued into the night. By the morning of April 7th, the Union reinforcements had arrived, and they now outnumbered the South by 10,000 men. The battle was won, and the Confederates retreated. But what was left was widespread battlefield carnage. The number of dead and wounded during the Battle of Shiloh was unprecedented. At that point in American history, there had never been anything like it. Over 3,000 soldiers from both sides were killed and more than 16,000 lay wounded. The medics had never seen such high numbers of wounded soldiers. It took over forty-eight hours just to retrieve the men from the field and tend to their wounds. Memoirs of soldier survivors tell of the chilly night and the heart-rending cries of the wounded in the dark. During the night, rain came, and the temperature dropped below freezing. The wounded lay in muddy, half-frozen puddles, anxiously awaiting their turn with the medic. Suffering was rife and hypothermia began to set in. Some soldiers had bullet wounds; others bayonet wounds. The open lacerations were contaminated by dirt and rainwater as they lay there in pain and filth for two days. During the night, some of the soldiers noticed a weak blue-green glow coming from their untreated wounds. As the medics tended to the soldiers, they began to notice a strange phenomenon that medical science had no answer for: the soldiers with glowing wounds had a much higher survival rate and were healing faster than those without glowing wounds. Everyone was puzzled. The germ theory of disease was not widely known or accepted during the 1860’s. The surviving soldiers referred to the phenomenon as Angel’s Glow. With thousands of soldiers dying all around them, their survival certainly felt miraculous. The story was passed down and eventually became a firmly rooted part of Civil War lore. It took nearly 140 years for the mystery of the glowing wounds to be solved. It involved Bill Martin, a 17-year-old high school student with an interest in the Civil War, and his mother, a research microbiologist working for the USDA. She studied luminescent bacteria found in soil. Bill remembered the story of the Battle of Shiloh and also knew about the glowing bacteria his mother studied. He was encouraged by her to find out if there was any connection between the two. He and his friend Jon Curtis visited the battle site and learned what they could about the battle conditions and the bacteria itself. They found that there are a few types of Photorhabdus luminescens bacteria that glow blue-green and digest microorganisms around them. These bacteria live in the guts of nematodes – tiny parasitic worms – and those worms hunt for insect larvae in soil. The microscopic nematodes burrow into the bodies of their insect larvae victims and then vomit up the P. luminescens bacteria, which then go on to produce chemicals that kill any microorganisms around it. The only problem, the boys found, was that the glowing bacteria cannot survive in the warm environment of the human body. They were stumped until they learned that weather conditions the night of the battle were cold and wet, and many of the soldiers were rescued from hypothermia. The colder temperatures of the soldier’s bodies would have been perfect for the glowing bacteria to thrive. The bioluminescent bacteria in the soldiers’ wounds killed all other nearby microorganisms - including ones that would have led to gangrene, and other often fatal infections common to that time. Because of the presence of the nematodes, and the glowing bacteria just going about their simple lives, the soldiers had their own little antibiotic factory working for them as they laid there waiting for help. Before they even reached the medic’s station, their wounds were cleaned, and healing had begun. They owed their very lives to those little glowing bugs.
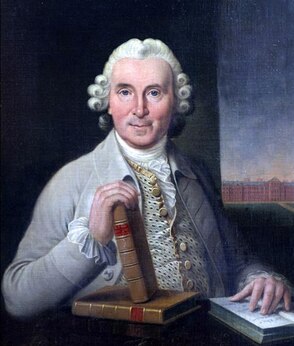
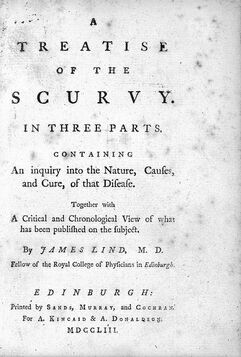
By: Courtney Southwick Imagine this scenario: It’s the 1700’s and you’re a sailor with the Scottish Royal Navy. You’ve been stuck on a ship for weeks and your shipmates are coming down with horrifying symptoms: bleeding gums, teeth falling out, shortness of breath, hallucinations, and eventual death. Food is getting scarce, and you trap a rat and eat it. Not many of the other sailors will eat the rats, but you’re feeling desperate enough. Every other ship coming back into port details the same dire situation: so much suffering and death. That scenario was tragically common for sailors back then – until James Lind came along. James Lind was not a doctor, though as a young teen he gained experience working as a surgeon’s apprentice. In the year 1740, the 24-year-old Lind boarded the HMS Salisbury, a 50-gun ship, as the surgeon’s mate. Britain was at war and each ship, and thousands of sailors, were needed. About six weeks out, sailors started getting sick around him, and Lind decided to investigate this strange disease that was crippling the Royal Navy. Over one six-year period, 18,500 sailors died: about ten percent of the enlisted. They needed a solution. We now know the disease the sailors were suffering from was scurvy, a simple vitamin C deficiency. Vitamin C is important; it helps with wound healing, collagen formation, the absorption of iron, and the formation and maintenance of tissues including bones, cartilage, and teeth. The usual first symptoms of scurvy are fairly generic: fatigue, soreness throughout the body, and stiff joints. But after that, your gums begin to swell and bleed, and your teeth loosen and fall out. Bleeding under the skin is next, and you can’t see it, but deep tissues begin to bleed as well. You experience swollen legs, anemia, hemorrhages, personality changes, apathy, and eventually death. It’s incredible that a simple vitamin can prevent all of that suffering. But back in James Lind’s time, vitamin C hadn’t been discovered yet, and the cause of scurvy was still a mystery. It wouldn’t be until the early 20th century that scientists discovered the existence and use of vitamins. In the 1740s, Lind assumed the symptoms he was seeing were evidence of a digestive disorder. On that ship, Lind went on to conduct what many scientists view as the world’s first clinical study. He took twelve sick men and divided them into six groups. He gave each group a different treatment every day for fourteen days. These treatments included: diluted sulphuric acid, vinegar, sea water, cider, a medicinal paste containing garlic and radish root, and lastly, citrus fruit: oranges and lemons. He checked on the progress of his patients daily and found that the men who were consuming the citrus fruits were healing and regaining their strength. The others were not. James Lind figured out how to treat scurvy. He did not know how or why the citrus fruits prevented and cured the terrible disease, but he knew they did. He published a book about it, but the notes of the clinical trial were lost in the 450-page behemoth. As is common with new discoveries, people did not want to believe it at first. He wasn’t a very good advocate for his work, and so for a while, not much changed. For years soldiers continued to die from scurvy; in fact, more died from scurvy than from wounds in battle. It took decades and the hard work of others, but finally in spring 1796, Great Britain’s Sick and Hurt Board – perhaps with the encouragement of the two sitting naval surgeons – announced that all ships on foreign service were required to carry lemon juice. That simple change drastically reduced scurvy cases, so three years later they announced the change for all British ships. Having all sailors eat the citrus fruits quickly led to the nickname of “Limey” that we occasionally still hear today. That was the end of scurvy in the navy. With lemon juice available to all sailors, health returned, and they were able to block French ports for years at a time, keeping Napoleon from invading Britain, and keeping Britain’s trade flowing freely. The simple addition of vitamin C through citrus fruits was so important to the viability of the navy that a lemon tree is included on the official crest of the British Institute of Naval Medicine.
James Lind might not have been the first to connect citrus fruits to scurvy, but he was the first to show its effectiveness through a randomized controlled trial. His scientific curiosity and compassion for those around him saved more lives than can be counted. And what is the significance of the sailor eating the rat? Most animals – including rats – synthesize their own vitamin C. Humans do not. Eating rats on the ship gave that brave and daring sailor a good dose of vitamin C and probably saved his life. |
Welcome to
my blog! I've been writing since I was twelve years old, and I fell in love with science in the 9th grade. In addition, I was raised by a writer and a historian, so I am here to combine my love of science, history, and writing. Join me here as I blog about the history of science and medicine. Archives |








 RSS Feed
RSS Feed